:max_bytes(150000):strip_icc():format(jpeg)/Health-GettyImages-CopperIUDSideEffects-9f6830fb6fcb4d239f0a9c8639615cc2.jpg)
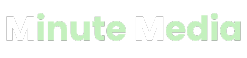
Copper IUDs are small, T-shaped devices inserted into your uterus to prevent pregnancy. The only available copper IUD in the United States is called Paragard.
Copper IUDs prevent sperm from reaching the uterus. They also cause an inflammatory response in the uterus. IUDs are among the most effective forms of birth control, with a 99% effectiveness rate.
Most people who use copper IUDs experience few side effects, but they’re still possible. People often choose copper IUDs when they can’t use hormonal IUDs or want to avoid typical hormonal IUD side effects like weight gain, mood swings, or sore breasts.
The most common copper IUD side effects include more painful menstrual cramps and heavier-than-normal menstrual bleeding. Though rare, copper IUDs may cause more serious side effects, such as uterine perforation and pelvic inflammatory disease.
Cramps and pain are among the top complaints of people who have copper IUDs. Increased cramps, along with heavier menstrual flow, are the top reasons why people choose to have IUDs removed, accounting for about half of all IUD removals.
You can typically alleviate cramping with over-the-counter (OTC) painkillers.
Heavier menstrual bleeding is more likely to happen with a copper IUD than a hormonal IUD. In fact, hormonal IUDs may reduce your menstrual bleeding.
Non-steroidal anti-inflammatory drugs (NSAID) pain relievers, like Advil and Motrin, can help reduce pain and can also potentially decrease menstrual bleeding.
Some people experience pain when the IUD is first inserted, though it’s less common among those who have delivered a baby vaginally. Do your best to choose a provider with proven experience inserting IUDs.
A healthcare provider will sometimes numb the cervix using an anesthetic before the IUD insertion to decrease pain. You can request this if you are concerned about pain.
Copper IUDs can sometimes increase your chances of a bacterial infection. This may occur if bacteria are introduced to the vagina during insertion. When this happens, you may experience a condition called bacterial vaginosis (BV), which is an imbalance of bacteria in the vagina.
Symptoms of BV include gray or fishy-smelling discharge, pain, and burning while peeing. BV can be treated with antibiotics. IUD removal is not usually necessary when this happens.
Though rare (roughly 2% of cases), IUDs can cause uterine perforation, which is damage or tearing to the uterus. Some research suggests hormonal IUDs are slightly more likely to cause uterine perforation than copper IUDs.
You probably won’t notice any symptoms of uterine perforation from your IUD—you just won’t be able to find the strings of the device. Treatment typically involves removing the IUD via laparoscopic surgery.
Pelvic inflammatory disease (PID) is a rare infection of the reproductive system, affecting about 2% of IUD users.
Pelvic inflammatory disease typically occurs during IUD insertion, when bacteria are introduced into the uterus. Antibiotics can successfully treat pelvic inflammatory disease.
Expulsion of the IUD is another less common side effect of copper IUDs. It occurs in about 5% of people within their first year of having an IUD. You may not notice the expulsion, but you will usually experience pain or bleeding or notice that the IUD has shifted.
You should see your provider if you suspect your IUD has moved. If you have symptoms, use other forms of birth control until the issue is addressed.
Though rare, it is possible to become pregnant with an IUD, occurring in only 0.6% of copper IUD users. If you have signs of pregnancy, including a missed period, you should contact your healthcare provider right away.
The most common side effects of copper IUDs, like pain, cramping, and bleeding, can be managed with medication and at-home remedies.
OTC pain relievers can help with pain. NSAIDs can help with pain and may also help decrease bleeding. You may also want to consider heating pads, warm baths, resting, and other at-home methods that you find useful when you have bad cramps.
If you experience a bacterial infection or pelvic inflammatory disease—both of which are rare—you will be treated with antibiotics. Your healthcare provider can effectively manage other rare side effects of copper IUDs. For instance, a perforated uterus can be treated with surgery.
For the most part, copper IUDs don’t cause long-term complications.
Some of the rare complications of copper IUDs can have consequences. For instance, 1 in 10 people who experience pelvic inflammatory disease become infertile. That’s why it’s vital to stay in touch with your provider if you have a copper IUD and get treatment for any infections that may arise.
If you get pregnant while using a copper IUD, your chances of having an ectopic pregnancy increase. Having a copper IUD makes it very unlikely that you will become pregnant in the first place, though, since the devices are 99% effective.
Besides decreasing the risks of unintended pregnancies, IUDs have other potential benefits. There’s evidence that both copper and hormonal IUDs can decrease the risk of uterine and ovarian cancer.
You may experience more cramps and bleeding when you have a copper IUD. It’s typically not an emergency, but you should feel free to talk with your healthcare provider about these side effects and options for managing them.
It’s not necessary to see your provider soon after your IUD insertion, but you should contact them if you have any of the following symptoms:
IUDs are birth control devices inserted into the uterus. There are two types of IUDs: copper and hormonal. Copper IUDs are a good choice for people who can’t use hormonal IUDs or wish to avoid the side effects of hormonal IUDs.
Most people don’t have side effects from copper IUDs, but side effects like menstrual bleeding and increased cramps are possible. While rare, copper IUDs can cause infections, uterine perforation, and expulsion.
If you have questions or concerns about your copper IUD, contact your healthcare provider as soon as possible.